It is privilege to write for this inaugural ISSHP newsletter.
Life’s perfect partnership starts with the placenta. If we get this right, we have the best chance of healthy life.
In preeclampsia, we have a failing placenta. Preeclampsia kills one pregnant woman every minute and the life expectancy of those who survive is greatly reduced. At the ISSHP2014 in New Orleans, I opened my talk by saying, “Preeclampsia is treated roughly the same way it was when Thomas Edison was making the first silent movie”. As an amateur poet, I was making a poetic statement. I don’t deny the improvements in the management of preeclampsia in prestigious hospitals in economically developed countries. Globally, millions of women risk death to give birth each year and almost 300,000 lose their life in this process. Over half a million babies around the world die each year as a consequence of preeclampsia. This is equivalent to every week twenty Airbus380 full of passengers falling from the sky. If this was happening, would you still be flying and would our governments remain in power?
Despite decades of research, why do we still lack pharmacological agents to treat it? Perhaps it is time for a new strategy. Dogma must give way to data. A historic symposium on ‘Novel Therapies for Preeclampsia’ took place at the ISSHP in New Orleans last year. I was honoured and humbled to be in such company. The ‘two-stage model’ of preeclampsia has served us well to make things clear but it is no longer fit for purpose. The attempt to modify it only helps to illustrate that it is becoming a ‘summary sheet’ of observations. Theories need to be tested, proven or discarded. We need to move beyond a “disease of theories”. British medical statistician, Austin Bradford-Hill listed the minimal conditions needed to establish a causal relationship between two items. When we applied the Bradford-Hill Criteria of Causation to preeclampsia research, we began to question many of the theories we had taken for granted. If you are interested, I refer you to a review entitled “Is inflammation the cause or consequence of preeclampsia?”
One thing is certain; maternal endothelial dysfunction is a central phenomenon responsible for the clinical signs of preeclampsia. The “why” is obvious, yet the “how” is unknown and crucially it is in the “how” that we will find therapies. In the late nineties, I discovered that vascular endothelial growth factor (VEGF) stimulated nitric oxide release. This led me to suggest that preeclampsia arises due to the loss of VEGF activity, possibly due to a rise in soluble Flt-1 (sFlt-1). Researchers in the US took the lead and showed that sFlt-1 elicited preeclampsia-like signs in pregnant rats and sFlt-1 increased before the clinical signs of preeclampsia in pregnant women. Around the same time, we demonstrated that removing or reducing this culprit protein from preeclamptic placenta restored the angiogenic balance. I would like to think this finding provided the conceptual evidence to pave the way for the development of therapeutic plasma apheresis, which removes sFlt-1 and improves clinical outcomes.
My goal had always been to rapidly develop new and affordable therapies for pregnancy complications that can be used globally with relative ease. Over the years I had lost sight of this mission, until one Spring day in 2006 while hiking on Malvern Hills in Worcestershire, Safia, my then ten year-old daughter asked “Daddy, you talk about VEGF all the time, but what have you really done?” This stunned me and led me to return to an old finding of mine on how to stop this disorder.
While most researchers focus on the causes of preeclampsia, I asked instead “why is it that 95% of pregnant women don’t get preeclampsia?” This was in the late nineties, when an enzyme called heme oxygenase-1 (HO-1 or Hmox1) that generates carbon monoxide (CO), biliverdin (rapidly converted to bilirubin) and iron, was being recognized as cytoprotective. I was able to show it prevented human placental injury caused by pro-inflammatory cytokines. After my daughter had brought focus to my life, I asked my PhD student to test whether HO-1 pathway suppressed sFlt-1 release. We demonstrated that CO inhibits two anti-angiogenic factors, sFlt-1 and soluble endoglin (sEng), responsible for preeclampsia phenotypes. This fits with the finding that women who smoke, but not those who chew tobacco, are protected from preeclampsia. I am not advocating smoking as therapy! The HO-1 / sFlt-1 theory meets the Bradford-Hill Criteria of causation.
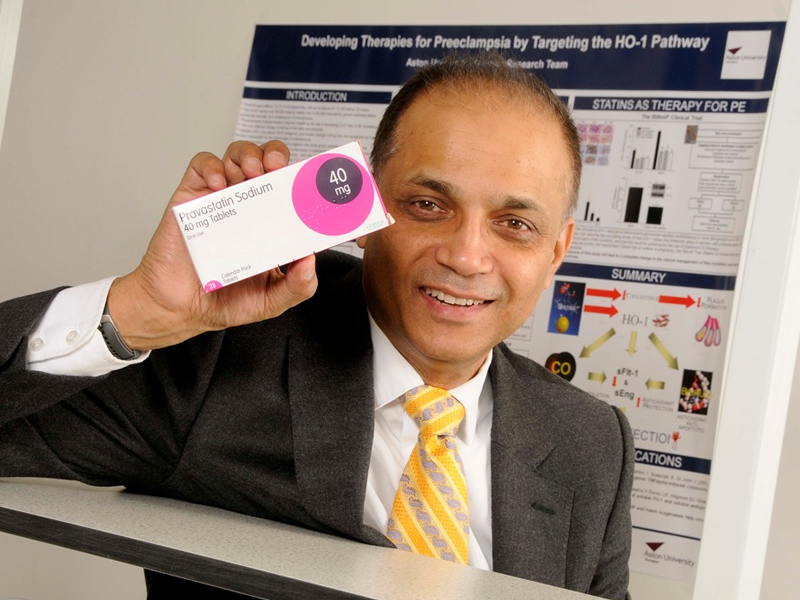
The other key enzyme we identified using this approach is the hydrogen sulfide (H2S) generating cystathionine-gamma-lyase (CSE or Cth). These are the only two enzyme systems shown to suppress sFlt-1 and to act as protective pathways against preeclampsia phenotypes in models. Our Circulation publication in 2013 showed that when hydrogen sulfide restores placental vasculature, it also improves lagging fetal growth. These molecules act as the inhibitor systems in pregnancy and when they fail, this triggers preeclampsia (see Figure 1). Discovering that statins induce these enzymes helped us to develop a low-cost therapy (StAmP Trial) to prevent or treat preeclampsia. Statins are contra-indicated in pregnancy, but following our Circulation paper of 2007, a flurry of animal studies began with statins. I took our cue from the 2002 Nobel Prize winner Professor Sydney Brenner, who in 2000 said, “Man is the experimental animal of the 21st century”. I opted for human studies and customized Sydney’s statement by saying; “Mother and Child are essential experimental subjects in the 21st century”.
If you think of pregnancy as a car then preeclampsia is an accelerator-brake defect disorder. Inflammation, oxidative stress and an imbalance in the angiogenic milieu fuel the ‘accelerator’. It is the failure in the braking systems (the endogenous protective pathway) that result in the ‘accelerator’ going out of control until the system crashes, manifesting itself as preeclampsia. A YouTube video commissioned by the British Council sums this up in three minutes: (http://youtu.be/vWUCWbKo1dE). The StAmP Trial is the starting point that employs this model. The strategy to identify a cure for preeclampsia needs to be centered on identification of drugs that up the braking system, reduces sFlt-1 and oxidative stress and are safe in pregnancy.
A son of a coal miner, Nye Bevan, gave us the NHS. He showed us that passion and focus could transform lives. It is a privilege to be leading the new Aston Medical School, whose goals are to promote social mobility in Medicine at a low cost to the public purse and research into women’s health and dementia. If we see a little further, it is only ‘by standing on the shoulders of giants’.
Professor Asif Ahmed
Pro-Vice-Chancellor for Health / Executive Dean, Aston University, Birmingham, UK.
E-mail: Asif.ahmed@aston.ac.uk ; Twitter: @ProfAsifAhmed
Asif Ahmed
Professor Asif Ahmed completed his BSc (1983) in Pharmacology from King¹s College and his PhD in Surgery (1989) from University College London. After a fellowship at the University of Cambridge, he took up a lectureship in 1993 at the University of Birmingham. He was rapidly promoted to Professor of Reproductive Physiology in 1998. He moved to the University of Edinburgh to take up the Gustav Born Chair of Vascular Biology, returning to Birmingham in 2012 as Pro-Vice-Chancellor for Health at Aston University, where he has developed a new model of medical education in England, with a focus on social mobility, delivered at low cost to the public purse. Professor Ahmed identified two enzyme systems as protective pathways against preeclampsia. Discovering that statins induce these enzymes, he initiated a low-cost therapy (StAmP Trial) to prevent or treat preeclampsia.